It is as incredible or even weird as it comes. According to Toronto Life, George Otto was a respected family physician with bustling clinic in the northwest corner of the city. But the magazine says Otto had a secret: after hours, he was running a booming Fentanyl business. Below are the lengthy but intriguing details of the untold story of the doctor who fuelled a drug crisis. More intriguing is how this could have gone on in a country such as Canada for the length of time involved.

Trained in History of International Relations at the LSE, the author teaches Journalism at Carleton University in Canada
By Brett Popplewell
In 2016, three decades after immigrating from Uganda, George Otto had the life he’d always wanted. He lived with his wife and four kids in the leafy, cushy gated community of Trailwood Estates in Richmond Hill. He’d bought his stone mansion in 2011 for $2.5 million. The house had six bedrooms, 10 bathrooms and a double-level five-car garage, where he parked his black Lexus.
Otto, who was 58, had worked hard to build his reputation as a trusted doctor in one of the city’s marginalized communities. At his clinic, located in a strip mall near Jane and Wilson, he was known for his comforting bedside manner. He spoke slowly and moved slowly, too. Many of his patients were new Canadians, and he spoke Swahili and Luo, which helped him forge connections with some of them. Otto treated any patient who entered his doors, whether or not they had OHIP. And he was paid very well: over one 16-month period, his billings totalled $803,858.
To his patients, Otto was a hard-working public servant who represented the embodiment of prosperity and generosity. As a student activist in Kampala, Uganda, he’d fled his home country to avoid the wrath of the military police, arriving in Canada as a political refugee in 1981. Later, once he’d established himself, he shared his success with others, granting free lodging to new immigrants arriving from Uganda—friends, friends of friends and extended family. He shipped textbooks back to his alma mater, Makerere University. And at the Uganda Martyrs United Church of Canada, he and his family were leading benefactors and vital members of the community. Yet he was also a show-off who liked to flaunt his fancy cars and entertain visiting Ugandan politicians and dignitaries at his impressive home. He seemed to thrive on ostentation—he was as gregarious as he was generous, and friends referred to the mansion as “Otto’s arena” because it was so big.
Every day, he drove 30 minutes south from Richmond Hill to his clinic, located next to a payday loan outlet. He’d pull into the lot, park his car and make his way inside. He’d turn on his computer and write patient charts before his first appointments started filing into the clinic at around 10 a.m. He often treated as many as 80 people in a 10-hour shift. Then, after he was done seeing patients for the day, he’d begin his other work. The work no one could find out about. The work that would destroy his life, along with hundreds of others.
Behind all his wealth and luxuries, Otto was hiding a secret. Back in the ’90s, when he was running a clinic at Kipling and Dixon, he’d simply stopped paying his taxes, for reasons he never fully explained. He eventually fell so far behind that he owed more than $375,000 in back taxes, plus an additional $190,000 in bank, student and personal loans. At the time, it wasn’t entirely clear how much he was making. He claimed he was bringing in just $2,400 per month in earnings—an inconceivably low sum for a family doctor. Instead of repaying his creditors, he opted to file for bankruptcy. For 15 years, between 1999 and 2015, Otto’s OHIP filings were garnished by $3,000 per month, going to the CRA and other creditors.
To maintain his lifestyle, Otto became embroiled in a scheme involving the province’s Special Diet Allowance, a program that provides up to $250 per month for patients who require special foods due to medical conditions. Otto falsified forms for patients who didn’t qualify, receiving $20 in service fees for each form he completed. As early as 2012, the College of Physicians and Surgeons, the governing body that regulates the medical profession in Ontario, investigated him, eventually ordering him to take a record-keeping course to clean up his paperwork. Two years later, they found that he was still overbilling the system. This time, they declared his actions disgraceful and dishonourable and fined him $10,000—a paltry sum, considering he’d collected at least $259,680 in service fees for the diet program.
But the college had no idea that he was partaking in a far more lucrative and dangerous scheme. That he’d found a way to earn as much as $9,000 a week under the table. All he had to do was write a few fentanyl prescriptions.

 The opioid crisis and the medical profession have been inextricably linked for the past 25 years. When OxyContin came on the market in the mid-’90s, it was prescribed as a panacea for any number of pain-related ailments. At the time, Canadian medical schools offered hardly any training on addiction medicine, and the medical profession was ill-informed about oxy’s deadly potential. The pharmaceutical companies, meanwhile, wielded even more control than the public knew: an inquiry in 2010 found that at least one pain-management course at U of T’s medical school was funded by grants from opioid companies between 2002 and 2006. A guest lecturer had also offered students a textbook published by the OxyContin manufacturer Purdue Pharma.
The opioid crisis and the medical profession have been inextricably linked for the past 25 years. When OxyContin came on the market in the mid-’90s, it was prescribed as a panacea for any number of pain-related ailments. At the time, Canadian medical schools offered hardly any training on addiction medicine, and the medical profession was ill-informed about oxy’s deadly potential. The pharmaceutical companies, meanwhile, wielded even more control than the public knew: an inquiry in 2010 found that at least one pain-management course at U of T’s medical school was funded by grants from opioid companies between 2002 and 2006. A guest lecturer had also offered students a textbook published by the OxyContin manufacturer Purdue Pharma.
In April 2012, the Ontario Ministry of Health and Long-Term Care created the Narcotics Monitoring System, or NMS, an automated database developed to stem the number of opioid scripts coming out of doctors’ offices in the province. The system automatically collects dispensing data from all Ontario pharmacies, ostensibly enabling the ministry to spot over-prescribers. The ministry then alerts the Ontario College of Pharmacists, which disciplines the offending pharmacists, as well as the College of Physicians and Surgeons of Ontario, which takes care of the doctors. The idea is admirable, but the execution is flawed: the colleges are meant to protect the public from their members, but both are self-governing and have been accused of protecting their own kind.
The NMS was designed to help prevent “double-doctoring” and “poly-pharmacy visits”—patients getting scripts from multiple doctors or filling their scripts at multiple pharmacies. But what happens when a bad doctor meets a bad pharmacist? The system wasn’t prepared for a scenario where the two collaborate to pump narcotics onto the street.
By 2014, the rules around oxy prescriptions had tightened—and a far more dangerous drug was supplanting it on the street. Doctors had gradually started prescribing transdermal fentanyl patches for their pain patients instead of oxy. A synthetic opioid, fentanyl is 50 to 100 times more powerful than morphine, heroin or oxy, but the transdermal patches release the drug into the bloodstream slowly. Theoretically, the risk of an overdose was lower—until, of course, people started placing several patches on their body at the same time, or even dismantling the patches and smoking, chewing or injecting what was inside. Like other opioids, fentanyl binds to receptors in the brain that control the body’s pain and emotions; over time, the brain relies on the drug in order to produce pleasure. Fentanyl’s sheer potency makes even the smallest exposure potentially deadly: a tiny amount of the drug could trigger an overdose in someone who’s never taken opioids before. As the drug took off on the street, dealers began selling both black-market prescription patches and fentanyl produced in underground labs. They mix the drug with heroin to produce a high so poisonous that even those patients who’ve built up a hefty opioid tolerance frequently overdose in parks, hospitals, hotel rooms, cabs and their homes. Between January 2016 and June 2020, the federal government recorded 17,602 apparent opioid-related deaths across Canada.
In Ontario, the medical profession has been reckoning with its role in the crisis for years. In 2016, the health ministry used the NMS to identify more than 80 doctors whose prescription practices far exceeded the standard of care, and the college launched an investigation into the over-prescribing crisis. The crackdown flushed out some of the bad doctors, and it terrified many others. Some physicians stopped prescribing opioids altogether, scared they’d get flagged by the system. As a result, many legitimate patients found themselves cut off from the pain drugs they needed.
Vincent Joel Rampton, an addictions and chronic pain specialist, was one of several physicians who worked closely with the college on its investigation. “We were part of [the crisis]…because OxyContin came along and we were misled [to believe] that it wasn’t as addictive as it was,” he later said. “There were a few physicians who were very out of control.”
 George Otto claims he never would have entered the illegal opioid trade if it weren’t for a pharmacist named Shereen El-Azrak. By March 2015, El-Azrak was spiralling from one crisis to another. She co-owned Weston PharmaChoice on Lawrence Avenue near Jane, and the doctor in the adjoining clinic had recently vacated his office. Like many pharmacists in Ontario, El-Azrak needed a physician nearby to write the prescriptions that would make up the backbone of her business. Otto had visited her pharmacy before, and she wanted to form a partnership. It was a common arrangement between doctors and pharmacists: she’d send him patients, he’d send her scripts.
George Otto claims he never would have entered the illegal opioid trade if it weren’t for a pharmacist named Shereen El-Azrak. By March 2015, El-Azrak was spiralling from one crisis to another. She co-owned Weston PharmaChoice on Lawrence Avenue near Jane, and the doctor in the adjoining clinic had recently vacated his office. Like many pharmacists in Ontario, El-Azrak needed a physician nearby to write the prescriptions that would make up the backbone of her business. Otto had visited her pharmacy before, and she wanted to form a partnership. It was a common arrangement between doctors and pharmacists: she’d send him patients, he’d send her scripts.
Life was difficult for El-Azrak. She had von Hippel–Lindau syndrome—a rare, painful condition that manifested in tumours that grew on her eyes, spinal cord and kidneys. The life expectancy for patients with the condition is 40 to 52 years. In 2015, El-Azrak was 37. She’d lost her vision in one eye and had required surgery to remove a tumour on her spine that had formed after the birth of her first child. At the same time, she was supporting her younger brother—who also had von Hippel–Lindau syndrome—and two kids, whose father lived in Cairo. They all shared an apartment at Yonge and Sheppard.
Before partnering with El-Azrak, Otto had never prescribed oxy or fentanyl. He knew that OxyContin was dangerously addictive, but had little awareness of fentanyl. He’d fallen behind on the medical literature and paid no attention to the warnings coming out of the college about its risks. When Otto partnered with El-Azrak, she sent scores of patients his way, many of whom were already hooked on fentanyl. Suddenly, Otto was prescribing patches to people he barely knew.
At some point after teaming up with Otto, El-Azrak brought him a new proposal. In recent months, she’d developed a lucrative side hustle, dispensing fraudulent fentanyl scripts. She worked with a few other doctors, who would write the scripts and pass them to drug dealers, who would sell them on the street. He could earn as much as $9,000 per week if he came on as a primary partner. Otto, no stranger to gaming the system, quickly agreed.
To distribute their product, Otto and El-Azrak worked with two dealers. The first was Liridon Imerovik, a 24-year-old high school dropout who went by the name Donny and lived in a basement apartment in Vaughan. El-Azrak employed Imerovik as a courier; since she was blind in one eye and unable to drive, he often chauffeured her to and from the pharmacy as well, and they’d become close confidantes. He’d been hooked on Percocet since 2010, when he and his father got into a serious car accident. Within four years, he was chewing 20 tablets a day.
The other dealer was Sean Holmes, an underemployed welder in Sudbury who’d begun dealing marijuana at age 12 and expanded his business in his teens and 20s. “He got addicted to fast money as a teen and to opioids as an adult,” says his father, Dene Holmes. By the time he teamed up with Imerovik, Holmes had developed such a high tolerance to fentanyl that he was consuming seven to nine 100-microgram transdermal patches every day, each one potent enough to kill an average adult.
The deal was simple. Otto would write a prescription for a box of 30 fentanyl patches, using names provided by Imerovik; they had to be real names so they could be logged in the NMS. El-Azrak would fill the prescriptions, then Imerovik would meet up with Holmes and exchange the drugs for cash. The patches would be stripped of their labels to avoid connecting them back to Otto or El-Azrak, and then, once back in Sudbury, Holmes would pass them on to a local barber who’d sell them from his house, charging roughly $350 per patch.
Both Otto and El-Azrak declined, through their lawyers, to participate in this story, but in court documents, they blamed each other to the end. Otto maintained that he had been duped into the scheme by El-Azrak, and El-Azrak presented Otto as the real mastermind. She claimed she just filled the scripts Otto gave her, no questions asked. For each script, Otto received $1,500 and El-Azrak $500. For his troubles, Imerovik received a retainer of $1,000 per week.
In June 2015 alone, Otto took home $33,000 from the scheme. The cash helped pay for the extravagant life he’d set up for himself and his family. It kept his jacuzzi hot and his Lexus fuelled. He had no idea who was using those fentanyl patches in Sudbury, who was overdosing, who was dying. Those people were so far removed from the life he’d built that they didn’t matter to him at all.
When summer hit, things got complicated. First, Imerovik was pulled over by Toronto police, who found on his person 30 fentanyl patches and a wad of cash. In his car, they found a handful of prescription receipts. Police also searched his apartment and discovered a debt list, 55 oxycodone tablets and some empty fentanyl packages made out in someone else’s name. He was charged with possession for the purpose of trafficking. Though the charges were later dropped, El-Azrak and Imerovik sensed the authorities were onto them. Desperate to keep a low profile, they tried to limit the prescriptions. Otto, it seemed, had also begun prescribing fentanyl to a number of new patients and dealers—people who were not directly associated with Imerovik’s operation. El-Azrak and Imerovik texted late into the night about how to convince Otto to pace himself and avoid detection. “He just wants more $$,” she wrote. “He does not realize what he is doing. I swear to god.”
But Otto had no intention of slowing down. He was on the college’s radar, but they only knew about the diet scheme, which had earned him a two-month suspension beginning in October 2015. Otto wanted to increase the number of weekly scripts from four to six, securing a further $3,000, likely to prepare for the losses he’d incur during his suspension.
In December 2015, two investigators from the Ontario College of Pharmacists showed up at El-Azrak’s drugstore, demanding access to her computer so they could pull the drug usage reports contained within—specifically for fentanyl. They’d found something peculiar: in the NMS, a handful of Otto’s prescriptions were numbered in sequence, but dated weeks or even months apart. The college had come to suspect that the dates had been manually manipulated to cover up the fact that El-Azrak was logging several scripts at once.
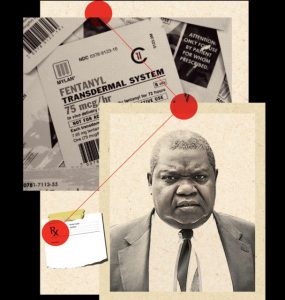
The closest to Dr George Otto’s face in the magazine as well as on the internet
Otto, meanwhile, had no idea anything was wrong. He treated his suspension like a holiday, travelling first to China and then to Uganda. He was still out of the country when the investigators knocked on El-Azrak’s pharmacy door.
When Otto returned from his suspension, business resumed as usual, and hundreds of fentanyl patches continued to flow out of Weston PharmaChoice. By this point, the opioid crisis was surging in Ontario: the number of annual opioid-related deaths in the province had nearly doubled over the previous five years, from 86 in 2010 to 162 in 2015. In Sudbury especially, deaths were on the rise, and police were trying to figure out how fentanyl was getting onto the streets. Around the time of Otto’s suspension and El-Azrak’s visit from the college, police got a tip that Sean Holmes was the primary source, and that he was bringing in drugs from the GTA. While Sudbury police monitored how the product was dispersed on the ground, York Region took over the main investigation.
Running the show was Detective Sergeant Nick Ibbott, a drug investigator with 27 years of experience on the force. After connecting Holmes to Imerovik, Ibbott and his team received warrants to track both their phones geographically and identify other numbers that contacted them. Over the next two months, they methodically pieced together Holmes’s supply line through a mix of on-the-ground surveillance and cellphone tracking. That’s how they discovered that the boxes of fentanyl patches Imerovik was selling to Holmes every week were coming out of a single pharmacy located in a North York parking lot between a Wendy’s and a Dollarama.
Week after week, police monitored as Holmes’s phone travelled 350 kilometres from Sudbury to Vaughan in its owner’s pants pocket. When the phone crossed into York’s jurisdiction, detectives would dispatch an unmarked tail to follow the phone to its destination, which tended to be one of several hotels off the 400. Holmes would check in to the hotel, stay in his room until late at night, then duck out and make his way to a rendezvous with Imerovik. On the first stakeout, police watched Holmes enter a Coffee Time with a duffel bag under his arm, then saw Imerovik emerge later carrying the same bag. The police monitored their meetups for the next two months. They knew exactly what they were witnessing, but they also knew that arresting Holmes would do nothing to shut down the source of the drugs. He was just a street dealer who wore flashy jewellery and baggy jeans—a pawn in a much larger operation.
In January 2016, the cops finally made their move. This time, police watched as a familiar-looking Jeep rolled into the parking lot of a Novotel in Vaughan. It was Imerovik. He walked through the lobby and made his way up to Holmes’s room on the third floor. Shortly after midnight, an undercover officer watched from the third-floor hallway as Imerovik exited Holmes’s room, carrying a flower-printed gift bag. That’s when Ibbott, monitoring the events from his base command centre, ordered his team to move in. Police arrested Imerovik and searched his car, finding $31,905 in the gift bag. In his pocket were two empty fentanyl boxes with prescription labels for two patients. In his car was a pile of forms, each of them for fentanyl patients receiving care from a Richmond Hill doctor named George Otto.
Imerovik was already on his way to jail when police knocked on Holmes’s hotel room door. Inside, they found 166 unmarked fentanyl patches with an estimated street value of $58,000. Before the night was out, officers headed across town to knock on El-Azrak’s door. She answered, accompanied by her young son, and was arrested immediately. They seized three cellphones, plus $18,000 in bundled cash from a dresser. By noon the following day, more than $75,000 in cash and roughly $89,000 worth of drugs were sitting in police custody.
When the forensic report from El-Azrak’s phones came in, Ibbott found himself staring at hundreds of pages of texts between her and Imerovik, and a complex web began to emerge, with a straight line leading back to Otto. Two months after the arrests of El-Azrak, Holmes and Imerovik, Ibbott finally had enough evidence to arrest Otto. The doctor had just parked his Lexus in a Home Depot parking lot when police approached him and read him his rights. By that point, he’d trafficked some 4,000 fentanyl patches onto the street.
It took three years for the figures at the centre of the Weston PharmaChoice fentanyl ring to make their way through the courts. Holmes was the first one tried, pleading guilty to a trafficking charge in 2017. He’d already spent time in prison on previous charges, and at his sentencing hearing, he broke down into tears and begged the court not to send him back—he was terrified he’d die of a drug overdose. “In 2010…I had never used fentanyl before,” he told the court. “One month in that institution I knew where to get fentanyl in that institution and out. I was putting needles in my arms every chance I got. I don’t want to die in prison…I’m asking you today to help me save my life.” Despite his pleas, he was sentenced to six and a half years in prison. Imerovik also pleaded guilty to two counts of trafficking fentanyl and one count of possession of fentanyl for the purpose of trafficking. He was sentenced to six years in jail. Imerovik’s lawyer, Randall Barrs, says the punishment was overly harsh. “Here was a guy who, through no fault of his own, became an addict,” he says. “As an addict, he got himself working for the pharmacy, and was under the thumb of the pharmacist.” By the time of his sentencing, Imerovik had managed to break his opioid addiction.
During El-Azrak’s eight-week trial in 2018, two conflicting stories emerged. The Crown portrayed her as a trained professional who knew full well the risks associated with opioid and fentanyl abuse, but who nonetheless chose to disregard her sense of decency to make some quick cash. The defence, meanwhile, depicted her as a tragic figure, easily manipulated by Imerovik and overcome by her own personal challenges. At one point, she became visibly upset on the stand describing the danger of the operation—how one time, a drug dealer had broken behind the counter to steal a box of narcotics, including some fentanyl patches. Justice Chris de Sa ultimately found El-Azrak guilty of both trafficking in fentanyl and possession of fentanyl for the purpose of trafficking, and sentenced her to 13 years in prison. “The breach of trust here is severe. Shereen is not an addict,” he explained. “Her only apparent motivation was greed.” El-Azrak is currently appealing her conviction.
Otto’s case didn’t reach the courts until 2019, and in the intervening time the College of Physicians and Surgeons launched an internal investigation against him, hiring a doctor on faculty at the University of Ottawa to examine the charts of 26 patients to whom Otto had prescribed fentanyl. In most cases, he found that Otto demonstrated a lack of judgment and skill in his prescription habits. He kept inadequate notes and “consistently prescribed doses of fentanyl in excess” of what would be considered normal for chronic pain management. In four of the 26 cases, Otto wasn’t able to present any patient charts whatsoever. The external reviewer found that Otto had a limited understanding of the standard of care. “Dr. Otto’s clinical practice and conduct is likely [to] expose patients to harm and injury,” he concluded. That document was filed with the college in May 2017.
Despite the college’s conclusions, Otto was permitted to keep treating patients and practising out of his clinic, though a court order forbade him from prescribing narcotics. Finally, in February 2019, he was suspended, and a month later he stopped paying his dues and let his membership lapse. In the end, the college nailed him not for drug trafficking, but for lousy record-keeping.

Sean Holmes, one of Otto’s main collaborators, helped distribute their illegal fentanyl patches
He spent the months leading up to his trial secluded in his Richmond Hill mansion. He told his friends not to worry about him. That once he got to trial he would be vindicated. He told them that the cops had it wrong. That he’d been a victim in all of this. That El-Azrak and Imerovik had conspired without his knowledge and that all he was trying to do was help people in pain.
Otto’s criminal trial finally began in June 2019. The Crown argued that he’d turned to trafficking fentanyl late in his career to deal with his financial struggles. The defence presented him as a hard-working doctor who’d treated as many as 33,000 patients, and who had no way of knowing that some of the scripts he was writing were being diverted to the black market. Over two days on the stand, Otto remained calm and collected, denying any wrongdoing and claiming he had no idea how or why a number of the scripts he’d written had ended up backdated in the NMS.
The jury didn’t buy it: they found Otto guilty of trafficking. At his sentencing hearing, Otto pleaded for leniency. “The last three years have been the most difficult time of my life. Ever. I have gradually lost my career since then. I have lost most of my social life that I had before because of what has been hanging over me, and I’m about to lose my personal freedom. I wish I’d never met Shereen.”
Justice Joseph Di Luca sentenced him to 12 years in prison. “A doctor, sworn by oath to help save lives, participated in a scheme that ultimately put many lives at risk. This tragic irony is made all the more acute when one considers that greed is the only apparent motive,” he said. “For reasons that are hard to fathom, Dr. Otto sacrificed his professional and personal existence to make easy money. Dr. Otto’s fall from grace is, in a word, staggering.”
During the trials, the names of five other doctors emerged—five doctors who were linked to El-Azrak and appeared to be trafficking fentanyl onto the street. And yet only Otto was ever charged with any wrongdoing. Like El-Azrak, he’s currently in the process of appealing his conviction.
Ibbott, who retired in 2019 after 30 years’ service, suggested that he knew there was a larger web of offenders, but his resources were limited. “If I had enough time, I could have taken out all the other potential doctors and traffickers,” he says. “But resources are always limited, and cases pile up. I don’t want to spiderweb an investigation where I have 1,000 people before the courts, because the courts are going to say, ‘Well, we’re going to deal with seven of them. So pick your favourite seven.’ ”
Until recently, the college was also limited in its disciplinary powers. Among the five doctors linked to El-Azrak’s practice, one was temporarily suspended and two have been verbally cautioned by the college; all three continue to practise in the GTA. One of the three—a professor emeritus with the University of Toronto—remains licensed, but is no longer allowed to prescribe narcotics. The other two doctors are no longer licensed, though not as a result of their opioid prescription practices. One source, who agreed to speak on the condition of anonymity, explains, “By and large, the college just wants to get bad doctors out in the fastest way possible. They’re less concerned with getting a scarlet letter onto the doctor’s profile.”
That Otto was permitted to keep treating patients despite the evidence against him is a testament to how broken the regulatory system was. At the time, the college didn’t have the power to suspend a licence without a hearing. A 2017 bill—the Protecting Patients Act—ostensibly changed that, empowering the college to immediately suspend doctors who were potentially putting patients at risk. When asked why Otto was permitted to continue practising despite the charges against him, the college said they couldn’t comment on specific cases, but suggested that their ability to take action is often complicated by the appeals process or the authorities’ ability to release information. The college explained that it’s continuing to re-evaluate its opioid strategy, updating it as recently as 2019. “This includes recent changes in reaction to fentanyl, increased access to prescribing history, and improving access to naloxone,” it explained.
Despite all efforts to crack down on Ontario’s opioid crisis, the death count continues to rise. Public Health Ontario estimated the province would close out 2020 with 2,271 opioid-related deaths—the vast majority of them accidental. That’s double the number of deaths in 2019.
On a snow-covered street corner next to Greater Sudbury City Hall, frozen wreaths and frozen flowers lie among more than 150 white crosses, each one representing an accidental opioid overdose in the city. One of those crosses represents Sean Holmes, Otto’s former collaborator.
After pleading guilty for his part in the drug trade, Holmes spent 18 months in prison, getting early release in December 2018. He did his time and paid his dues. For the better part of two years, he kept up with both his parole officer and his dad. “Sean was on a good path,” Dene Holmes says. Summer came, and the two spent most of their days at a cabin, catching up on lost time. Then, last fall, Sean relapsed. There was nothing he could do to save himself. One evening last September, he climbed into his truck and went to sleep. That night, he died of a fentanyl overdose.